Health plans who do not provide optimal Formulary and Benefit (F&B) information to prescribers through Electronic Health Records (EHRs) are missing a significant opportunity to lower medication costs and increase patient adherence to treatment.
Even for health plans that use Pharmacy Benefit Managers (PBMs), many prescribers only receive basic formulary information through their EHRs, leaving them without the necessary details to prescribe clinically effective drugs that patients can afford. Without access to robust formulary and benefit information, prescribers lose time selecting appropriate drug treatments, health plans pay for non-preferred prescriptions, and patients are more likely to abandon prescriptions they cannot afford.
Many are pointing to the future with real time pharmacy benefit information in the EHR. The combination of formulary and benefit information to inform a prescriber’s initial choice and real time pharmacy benefit information to affirm the prescriber’s selection may be the most optimal process to save prescribers time while selecting the most cost-effective medication for the patient. However, real time benefit information is in its infancy with many EHRs yet to include new this new information and additional delays by practices to decide to activate the feature. This process may take years and require multiple connections to receive data from all payers. Enhancing formulary and benefit data is here today and is available in virtually every EHR. Health plans can activate the following and receive the benefit quickly without much action on the part of EHR users.
Integrating a Solution within Existing Infrastructure: 3 Steps to Take Now
Less sophisticated formulary & benefit data can be supplemented to provide prescribers with actionable information at the point of prescribing. Health plans that rely on basic formulary information from PBMs have an opportunity to benefit from supplementing existing PBM data to physicians through EHRs and receiving the benefits of these investments. Here are three steps health plans can take now to augment elementary F&B data in EHR systems:
#1 Include Copay Information
When prescribers have access to copay information, preferably dollar and/or percent copays versus tier levels, they can discuss prescription costs with patients and estimated pharmacy costs. Copays aid prescribers to avoid cost-prohibitive prescriptions and select more affordable options. It also helps patients avoid sticker shock when they pick up their medication, reducing the number of callbacks and prescription revisions for prescribers. Finally, copays can indicate mail order savings and if a preferred retail pharmacy is available. F&B information can accommodate most copay structures with technology standards that exist today.
#2 Include Drug Alternatives
Health plans that supplement F&B data with clinically equivalent alternatives information can realize significant savings while supporting patient affordability and adherence. Providing alternatives assists physicians with selecting cost-effective brands and can aid in choosing lower-cost generics even when multiple generic options are available. Better results will be achieved with a shorter, more actionable list of clinical alternatives versus a full therapeutic list of potential alternatives.
#3 Provide Clinical Edits and Message Physicians with Clinical Drug Information
With electronic prior authorization (ePA) becoming a standard practice, plans need to provide accurate prior authorization indicators. By proactively informing physicians of the need for a PA, they can determine if another medication can meet their patient’s needs without the administrative hassle of obtaining authorization.
Adding the ability to provide prescribers with relevant clinical messaging helps them make the most informed choice for their patients’ needs. For instance, integrating messaging functionality enables health plans to notify doctors about appropriate drug use, drugs that have risk alerts, and drugs with important clinical information prescribers need when writing prescriptions. Even limits on quantity and frequency can be included in the message.
With electronic prior authorization (ePA) becoming a standard practice, providing accurate prior authorization indicators is another clinical message that may need attention. Today, too many drugs are missing PA flags which is a major reason why the number of ePAs run through EHRs continues to be underwhelming. An effort to improve PA flags in formulary data would be welcomed by stakeholders who need prospective PA flags to drive the ePA process. By proactively informing physicians of the need for a PA, they can determine if another medication can meet their patient’s needs without the administrative hassle of obtaining authorization.
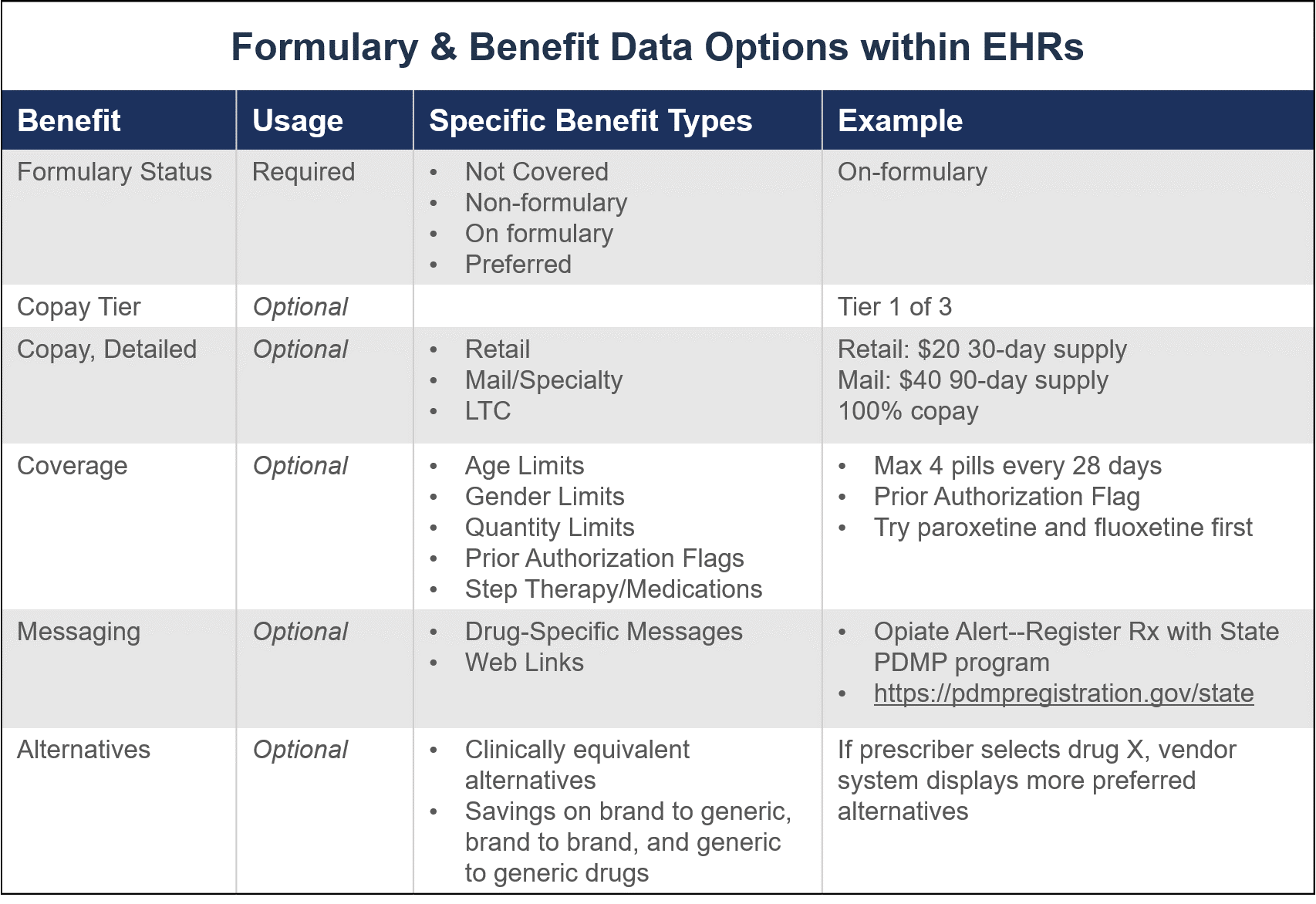
The National Council for Prescription Drug Programs (NCPDP) develops and promotes standards that determine the information available to prescribers within EHRs. Use of the standard is required for Medicare Part D plans. While formulary status is required, other information that enhances the prescriber’s ability to make informed prescription decisions is optional.
Cost and Timeframe Considerations for Improved Data
The good news is that patient formulary information such as copays, alternatives, and coverage information like prior authorization requirements can be provided through existing EHR infrastructure quickly and efficiently.
The cost of implementing additional data into existing PBM data is modest compared with the potential savings for most health plans. The flow from PBMs to EHR to physicians is well-established and available at little to no additional cost. While the update timing varies from one EHR to another, information will generally appear in most systems within a month.
A 2018 Benmedica study of one million members analyzed over 13 million claims representing $1.24B in drug spend revealed that when managed drug alternatives information and their cost are included in EHR data, the potential savings across eight evaluated therapeutic classes averaged $6.21 per member per month with 100% adoption. While 100% adoption is exceptionally unlikely, the potential of realizing a significant savings is strong, especially in conjunction with provider contracts and training.
Learn How We Help Health Plans Save Money Through Better Formulary Information
Benmedica helps health plans optimize EHR data so that prescribers can select the best, most affordable medications for their patients. Our work lowers patient costs, saves health plans time and money, and supports patient adherence. Contact us today to learn how much you can save by providing better information to prescribers at the point of care.