Proactive work on the part of payers can make drug alternatives that appear in EHRs Electronic Health Record systems (EHRs) more useful and resolve differences between alternatives displayed using Formulary & Benefit (F&B) and those that appear in Real-Time Pharmacy Benefit (RTPB) information.
Increasing the relevance and consistency of alternatives is critical for adoption by prescribers. Acceptance and usage of the alternatives by prescribers will assist patients and payers in lowering drug costs through better drug selection and will increase patient satisfaction with their health plan.
Without credible alternatives displayed in the EHR during the prescribing process, payers fail to offer a significant feature within F&B, which could help reduce drug costs for their members and alleviate prescriber alert fatigue.
EHRs can provide alternative information from both Formulary & Benefit information and from Real-Time Pharmacy Benefit (RTPB) information (sometimes called Real-Time Benefit Tools or RTBT). F&B is displayed as part of the prescription writing process, most often when selecting a drug from the provider favorites list or doing a drug search
For example, if the prescriber selects Dexilant then screen below appears. Note that the screens in this article are mock-ups to reflect how an EHR may display the e-prescribing process. They are simulacrums of what prescribers are currently using.
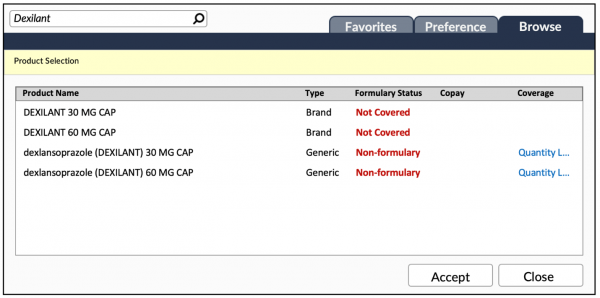 Note that neither Dexilant nor its generic equivalent is a preferred product. If the prescriber proceeds to select the dexlansoprazole (DEXILANT) 30 MG CAP option, then an alternatives drug screen (or an area on the current screen, depending on the EHR’s user interface) will appear.
Note that neither Dexilant nor its generic equivalent is a preferred product. If the prescriber proceeds to select the dexlansoprazole (DEXILANT) 30 MG CAP option, then an alternatives drug screen (or an area on the current screen, depending on the EHR’s user interface) will appear.
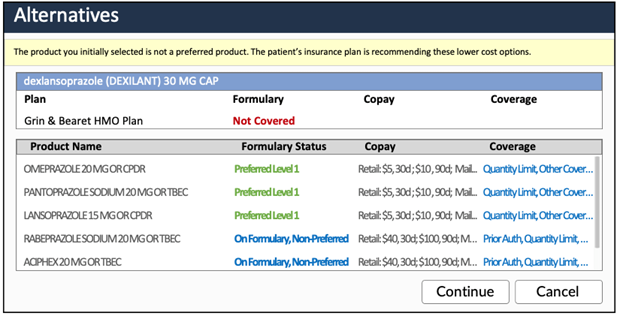
The image shows a list of drug alternatives that are therapeutically similar to dexlansoprazole 30 MG capsules and can be easily interchanged.
A much more common view of alternatives is by therapeutic class.
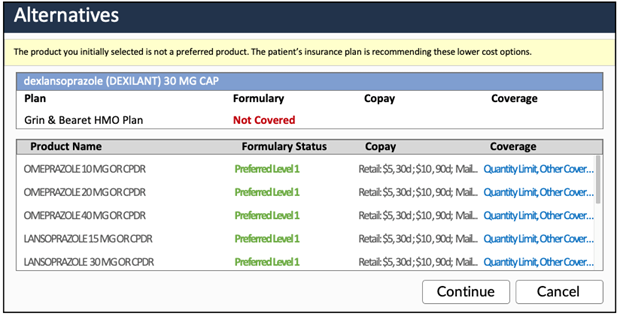 This screen is a list of alternatives by therapeutic class. It shows all drugs that have a better formulary status and are in the same therapeutic class as dexlansoprazole/Dexilant. It’s a longer list and does not provide equivalency which requires the prescriber research which strength is similar to dexlansoprazole 30 mg.
This screen is a list of alternatives by therapeutic class. It shows all drugs that have a better formulary status and are in the same therapeutic class as dexlansoprazole/Dexilant. It’s a longer list and does not provide equivalency which requires the prescriber research which strength is similar to dexlansoprazole 30 mg.
 If the prescriber decides to proceed with dexlansoprazole 30 MG capsules, then the next steps will be to complete the prescription. To run a proper RTPB transaction, the pharmacy, quantity and day supply will need to be entered.
If the prescriber decides to proceed with dexlansoprazole 30 MG capsules, then the next steps will be to complete the prescription. To run a proper RTPB transaction, the pharmacy, quantity and day supply will need to be entered.
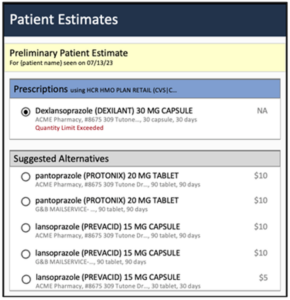
Just before the script is submitted to the pharmacy, the EHR may automatically run an RTPB transaction, or the prescriber can run a RTPB. A RTPB transaction may return a similar screen to this one.
For RTPB, if the PBM does return alternatives, then the alternatives will likely be therapeutically similar like the first F&B alternatives screen. Because RTPB is supposed to display with minimal latency, the number of alternatives is typically limited to around 5 (though there can be up to 9 based on the version of RTPB used).
The PBM’s adjudication engine must price each alternative then sort the results in real-time. For a PBM, performance and system stress limit the number of alternatives sent. Note that the PBMs often provide 90-day cost savings options (retail and mail order). It’s a balance between the number of alternatives, pharmacy options and cost savings. The PBM may focus on fewer alternatives but more pharmacy options to reduce drug costs, but it also reduces the number of drug options. In the example above, only two drugs are provided and most at the 90-day supply.
These two sources can conflict when they display different alternatives causing provider frustration. As we stated in our previous article Physician Perspectives of Real Time Pharmacy Benefit Tools a recent study that interviewed physician users of RTBT information found that the information appeared after the discussion with the patient about adding a proposed new medication to the patient’s treatment plan. Any prescription changes required the prescriber to re-evaluate the medication selected and adjust the prescription after the fact.
Formulary & Benefit implementation rules in place with virtually all EHRs require that when a non-preferred drug is selected by the prescriber that alternatives appear. If those alternatives are not provided by the payer or PBM then the EHR uses their drug database to select similar drugs within the original drug’s therapeutic class and with better formulary coverage as alternatives.
Another 2022 JAMA publication, Effects of Real-time Prescription Benefit Recommendations on Patient Out-of-Pocket Costs, indicated that only 4.2% of prescriptions were seen to have an available alternative. The alternatives led to an 11.2% reduction in costs. In high-cost drug classes the savings were more dramatic at 38.9%. Ensuring that the information provided is relevant and consistent throughout the process will help prescribers to find value of the information.
Issues With Simple Alternatives
Our review of the literature and discussions with organizations that use F&B and RTPB tools have identified the following challenges with alternatives. Here’s what our analysis found:
The result of these challenges is a less than ideal prescriber experience and result in higher drug costs for patients with missed savings for payers and PBMs.
Let’s review the full drug alternatives comparison in greater detail from the previous screenshots.
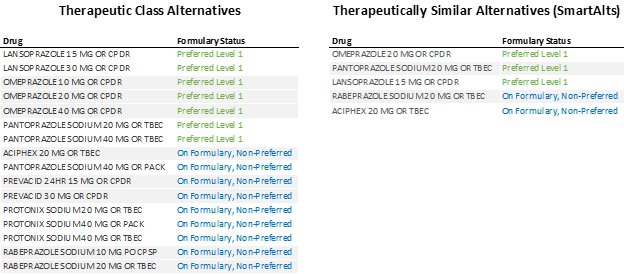 When the alternatives are expanded for each option, it becomes clear that the therapeutic class alternatives provide some guidance but still require additional effort by prescribers to scroll through the options and determine strength similarity. In addition, some valid alternatives may not be listed if the alternative drug is not in the same therapeutic class.
When the alternatives are expanded for each option, it becomes clear that the therapeutic class alternatives provide some guidance but still require additional effort by prescribers to scroll through the options and determine strength similarity. In addition, some valid alternatives may not be listed if the alternative drug is not in the same therapeutic class.
Therapeutically similar alternatives like Benmedica’s SmartAlts™ make the alternative drug list significantly more useful by being succinct, overcoming the therapeutic class alternatives limitations.
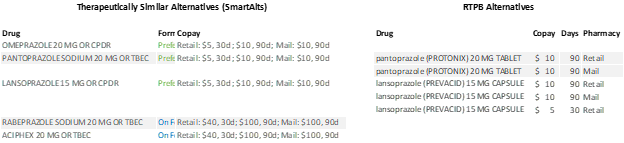 In this comparison, we see that F&B provides a larger number of chemically distinct alternatives as well as the copay for each pharmacy type. It’s the equivalent of 15 RTPB responses. In addition, F&B would provide additional coverage information details (not shown to keep reduce horizontal space).
In this comparison, we see that F&B provides a larger number of chemically distinct alternatives as well as the copay for each pharmacy type. It’s the equivalent of 15 RTPB responses. In addition, F&B would provide additional coverage information details (not shown to keep reduce horizontal space).
Drug database companies have excellent services that among many other functions, categorize drugs. Those drug databases are a fine starting point for identifying alternatives, but the databases aren’t privy to formulary statuses and net cost information that payers and PBMs have at their disposal. This is where careful planning of alternatives come into play. Benmedica offers SmartAlts™ service which when combined with formulary and cost information can enhance drug alternatives that appear in both F&B and RPPB data.
While providing valued and consistent alternative drug suggestions remains a challenge today, we believe that the solution lies in supplying better information to prescribers. Benmedica is on the forefront of creating, reviewing, and augmenting drug coverage information, including alternatives, so that employers and payers can use robust information to ease the physician prescription-selection burden while improving relationships with patients.
If you have questions, contact us to discuss how we can help your organization improve alternatives with our SmartAlts™ service please contact the Benmedica team today.