By Bryan Odegard, CEO, Benmedica
Artificial Intelligence (AI) dominates headlines in healthcare from Nvidia’s strategic expansion into medical AI, to policy volatility shaking up biotech investment. But beneath the noise lies a quieter, more foundational opportunity:
At Benmedica, we believe this is where AI becomes transformational and not by adding another dashboard or predictive widget, but by reshaping how core workflows operate. That’s where clinical, financial, and administrative friction is reduced. That’s where smarter decisions happen.
While the industry buzz often focuses on precision diagnostics, genomics, or wearables, the true ROI of AI comes when it's embedded into the information infrastructure of healthcare operations.
When application-layer AI is integrated directly into platforms, benefits logic, and real-time data structures, the results are measurable:
AI doesn’t just speed up decisions—it can contextualize them. In a 2024 survey by BMC Digital Health, 84% of institutions reported using AI for decision support in clinical workflows, citing improved efficiency and patient flow as top benefits.
This is not automation for automation’s sake. It’s workflow-aware intelligence which is designed to recognize formulary nuance, plan design, and patient-specific cost dynamics.
Take Nvidia’s recent positioning in healthcare AI. Their focus isn’t only on imaging and diagnostics but on how their AI infrastructure integrates into data platforms used by hospitals and researchers alike. That same principle applies to benefit intelligence. We believe prescribing, benefit verification, and plan-aligned recommendations must be augmented by the same embedded intelligence and delivered at the right point in the care journey.
This is the foundation we’re building with BenCore™.
Innovation without integrity is a risk. As AI expands across healthcare ecosystems, governance and model fidelity are no longer optional but rather foundational.
At Benmedica, our platform vision is grounded in these principles. Any intelligence introduced into our system must be trusted, explainable, and rigorously reviewed because trust is the only real foundation for scalable impact in healthcare.
Even as policy shifts and market dynamics evolve, one thing remains clear:
Efficiency at the core beats novelty at the edge.
The future of care isn’t just faster. It’s smarter by design.
We’re focused on operationalizing that future through accountable infrastructure, embedded intelligence, and aligned partnerships. That’s where innovation becomes real.
📚 Referenced Sources
The industry has made strides with ePrescribing but static formulary data, inconsistent alternatives, and disconnected RTPB transactions still limit outcomes for patients, plans, and providers. The opportunity? Make the data smarter, clearer, and more actionable.
That’s the power of Benmedica’s BenCore™ Medication Benefit Insights platform, starting with its BenCore eRx+™ Integration Suite, built to enhance the data powering prescribing decisions without requiring full system overhaul.
BenCore eRx+™ module adds intelligence, clarity, and clinical value where it matters most:
Precision F&B™
Intelligent RTPB™
Too often, v60 is viewed as a standards update. But in reality, it’s an opportunity to improve plan adherence, lower costs, and eliminate unnecessary barriers.
Benmedica helps organizations not only comply but thrive with v60 through:
"Let’s turn your compliance milestone into a strategic advantage."
(Source: Point-of-Care Partners Whitepaper: From Ignored to Impactful, 2024)
Whether you’re a health plan optimizing cost and adherence, a PBM enhancing your infrastructure, or a plan sponsor seeking ERISA-compliant transparency, BenCore’s eRx+ and v60 readiness unlock immediate value.
Learn more: Contact Benmedica
At Benmedica, we call this “savings by a thousand cuts”- the incremental, often-overlooked savings opportunities that, when combined, create meaningful financial impact across the healthcare system.
Recent research highlights the urgency of addressing prescription drug costs. Studies show that switching from high-cost generics to lower-cost therapeutic alternatives can reduce spending by up to 88% while maintaining clinical efficacy.¹ Meanwhile, a formulary-driven study found that such substitutions cut total drug costs from $7.5 million to approximately $873,711, demonstrating the power of incremental savings.²
Real-world data from health plans using Benmedica’s SmartAlts® solution demonstrates significant cost savings, with over $90 million saved in the first eight months - including $6.5 million in the first month alone—driven by seamless provider adoption. Further analysis shows that nearly half of these savings came from high-volume, lower-cost drug alternatives, highlighting the powerful impact of data-driven formulary optimization in reducing costs while maintaining clinical effectiveness.
Beyond Big Savings: The Power of Small Wins
Traditional cost-saving strategies tend to prioritize high-cost drugs with the largest price tags. However, this approach leaves substantial savings on the table by overlooking smaller but frequent opportunities that create a major cumulative impact. Consider:
✔ Lower-cost alternatives in widely prescribed drug classes (e.g., antibiotics, antihypertensives, cholesterol medications) generate massive cumulative savings across a population.
✔ Therapeutic substitutions in less-targeted categories (e.g., dermatology, gastrointestinal drugs) uncover hidden savings that would otherwise go unnoticed.
By making these small, consistent optimizations, payors, PBMs, and health plans can scale incremental savings into measurable financial and operational benefits. A recent analysis demonstrated that shifting just 5% of prescriptions to lower-cost alternatives in a 500,000-member health plan resulted in millions in annual savings.³
Unveiling Hidden Value with SmartAlts®
Benmedica’s SmartAlts® engine is built to unlock and deliver these hidden savings opportunities at scale. With a robust dataset of 18,000 drugs and 1,200 subsets of therapeutically similar alternatives, and proprietary clinical algorithms, SmartAlts® ensures cost-effectiveness without compromising clinical outcomes.
How SmartAlts® Drives Savings:
✔ Comprehensive Drug Class Analysis – Goes beyond high-cost drugs to identify savings in all therapeutic areas.
✔ Real-Time, Actionable Insights – Embeds data-driven alternatives directly into prescribing workflows.
✔ Compounding Cost Reduction – Small medication shifts (brand to generic, generic to lower-cost alternative) accumulate into major savings.
Case in Point: In a recent formulary adjustment, switching Budesonide-Formoterol to Symbicort as a preferred option resulted in $465,000 in savings within five months, proving that even minor changes can have a dramatic financial impact.³
Why Drug Alternatives Matter More Than Ever
The POCP Whitepaper highlights how traditional formulary management strategies have historically been static and underutilized, providing limited visibility into cost-effective alternatives. SmartAlts® changes this by embedding intelligent drug alternatives directly into prescriber workflows, reducing friction, improving adherence, and optimizing drug spend at scale.³
Transforming Small Wins into Big Results
At Benmedica, we believe that hidden value in drug alternatives is too important to ignore. Savings by a thousand cuts isn’t just a concept - it’s a strategic approach to drug benefit optimization.
With SmartAlts®, health plans, PBMs, and employers can tap into millions in savings while improving provider and member experiences.
Are you ready to unlock the hidden savings within your medication benefits? Contact us today to learn how Benmedica’s SmartAlts® solutions can help.
Proactive work on the part of payers can make drug alternatives that appear in EHRs Electronic Health Record systems (EHRs) more useful and resolve differences between alternatives displayed using Formulary & Benefit (F&B) and those that appear in Real-Time Pharmacy Benefit (RTPB) information.
Increasing the relevance and consistency of alternatives is critical for adoption by prescribers. Acceptance and usage of the alternatives by prescribers will assist patients and payers in lowering drug costs through better drug selection and will increase patient satisfaction with their health plan.
Without credible alternatives displayed in the EHR during the prescribing process, payers fail to offer a significant feature within F&B, which could help reduce drug costs for their members and alleviate prescriber alert fatigue.
EHRs can provide alternative information from both Formulary & Benefit information and from Real-Time Pharmacy Benefit (RTPB) information (sometimes called Real-Time Benefit Tools or RTBT). F&B is displayed as part of the prescription writing process, most often when selecting a drug from the provider favorites list or doing a drug search
For example, if the prescriber selects Dexilant then screen below appears. Note that the screens in this article are mock-ups to reflect how an EHR may display the e-prescribing process. They are simulacrums of what prescribers are currently using.
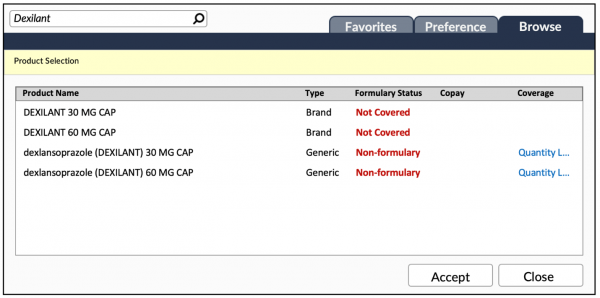 Note that neither Dexilant nor its generic equivalent is a preferred product. If the prescriber proceeds to select the dexlansoprazole (DEXILANT) 30 MG CAP option, then an alternatives drug screen (or an area on the current screen, depending on the EHR’s user interface) will appear.
Note that neither Dexilant nor its generic equivalent is a preferred product. If the prescriber proceeds to select the dexlansoprazole (DEXILANT) 30 MG CAP option, then an alternatives drug screen (or an area on the current screen, depending on the EHR’s user interface) will appear.
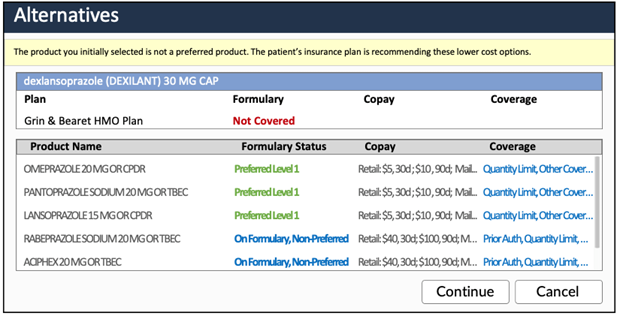
The image shows a list of drug alternatives that are therapeutically similar to dexlansoprazole 30 MG capsules and can be easily interchanged.
A much more common view of alternatives is by therapeutic class.
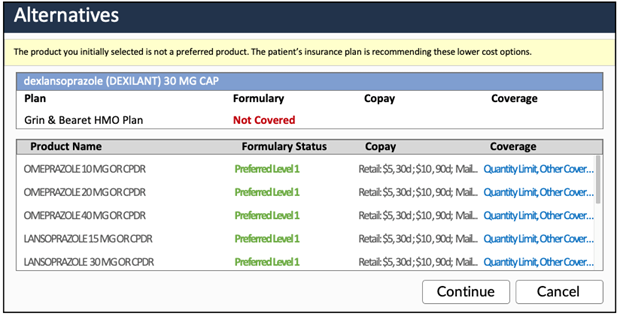 This screen is a list of alternatives by therapeutic class. It shows all drugs that have a better formulary status and are in the same therapeutic class as dexlansoprazole/Dexilant. It’s a longer list and does not provide equivalency which requires the prescriber research which strength is similar to dexlansoprazole 30 mg.
This screen is a list of alternatives by therapeutic class. It shows all drugs that have a better formulary status and are in the same therapeutic class as dexlansoprazole/Dexilant. It’s a longer list and does not provide equivalency which requires the prescriber research which strength is similar to dexlansoprazole 30 mg.
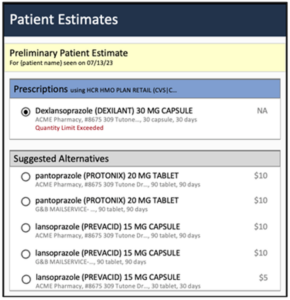 If the prescriber decides to proceed with dexlansoprazole 30 MG capsules, then the next steps will be to complete the prescription. To run a proper RTPB transaction, the pharmacy, quantity and day supply will need to be entered.
If the prescriber decides to proceed with dexlansoprazole 30 MG capsules, then the next steps will be to complete the prescription. To run a proper RTPB transaction, the pharmacy, quantity and day supply will need to be entered.
Just before the script is submitted to the pharmacy, the EHR may automatically run an RTPB transaction, or the prescriber can run a RTPB. A RTPB transaction may return a similar screen to this one.
For RTPB, if the PBM does return alternatives, then the alternatives will likely be therapeutically similar like the first F&B alternatives screen. Because RTPB is supposed to display with minimal latency, the number of alternatives is typically limited to around 5 (though there can be up to 9 based on the version of RTPB used).
The PBM’s adjudication engine must price each alternative then sort the results in real-time. For a PBM, performance and system stress limit the number of alternatives sent. Note that the PBMs often provide 90-day cost savings options (retail and mail order). It’s a balance between the number of alternatives, pharmacy options and cost savings. The PBM may focus on fewer alternatives but more pharmacy options to reduce drug costs, but it also reduces the number of drug options. In the example above, only two drugs are provided and most at the 90-day supply.
These two sources can conflict when they display different alternatives causing provider frustration. As we stated in our previous article Physician Perspectives of Real Time Pharmacy Benefit Tools a recent study that interviewed physician users of RTBT information found that the information appeared after the discussion with the patient about adding a proposed new medication to the patient’s treatment plan. Any prescription changes required the prescriber to re-evaluate the medication selected and adjust the prescription after the fact.
Formulary & Benefit implementation rules in place with virtually all EHRs require that when a non-preferred drug is selected by the prescriber that alternatives appear. If those alternatives are not provided by the payer or PBM then the EHR uses their drug database to select similar drugs within the original drug’s therapeutic class and with better formulary coverage as alternatives.
Another 2022 JAMA publication, Effects of Real-time Prescription Benefit Recommendations on Patient Out-of-Pocket Costs, indicated that only 4.2% of prescriptions were seen to have an available alternative. The alternatives led to an 11.2% reduction in costs. In high-cost drug classes the savings were more dramatic at 38.9%. Ensuring that the information provided is relevant and consistent throughout the process will help prescribers to find value of the information.
Issues With Simple Alternatives
Our review of the literature and discussions with organizations that use F&B and RTPB tools have identified the following challenges with alternatives. Here’s what our analysis found:
The result of these challenges is a less than ideal prescriber experience and result in higher drug costs for patients with missed savings for payers and PBMs.
Let’s review the full drug alternatives comparison in greater detail from the previous screenshots.
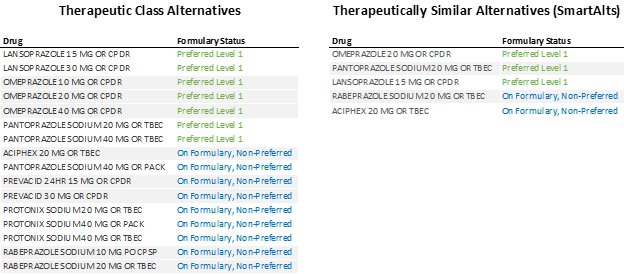 When the alternatives are expanded for each option, it becomes clear that the therapeutic class alternatives provide some guidance but still require additional effort by prescribers to scroll through the options and determine strength similarity. In addition, some valid alternatives may not be listed if the alternative drug is not in the same therapeutic class.
When the alternatives are expanded for each option, it becomes clear that the therapeutic class alternatives provide some guidance but still require additional effort by prescribers to scroll through the options and determine strength similarity. In addition, some valid alternatives may not be listed if the alternative drug is not in the same therapeutic class.
Therapeutically similar alternatives like Benmedica’s SmartAlts™ make the alternative drug list significantly more useful by being succinct, overcoming the therapeutic class alternatives limitations.
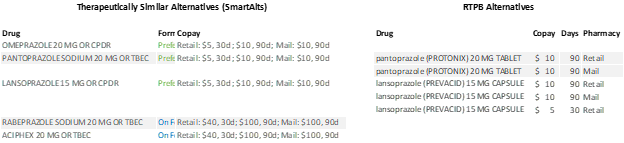 In this comparison, we see that F&B provides a larger number of chemically distinct alternatives as well as the copay for each pharmacy type. It’s the equivalent of 15 RTPB responses. In addition, F&B would provide additional coverage information details (not shown to keep reduce horizontal space).
In this comparison, we see that F&B provides a larger number of chemically distinct alternatives as well as the copay for each pharmacy type. It’s the equivalent of 15 RTPB responses. In addition, F&B would provide additional coverage information details (not shown to keep reduce horizontal space).
Drug database companies have excellent services that among many other functions, categorize drugs. Those drug databases are a fine starting point for identifying alternatives, but the databases aren’t privy to formulary statuses and net cost information that payers and PBMs have at their disposal. This is where careful planning of alternatives come into play. Benmedica offers SmartAlts™ service which when combined with formulary and cost information can enhance drug alternatives that appear in both F&B and RPPB data.
While providing valued and consistent alternative drug suggestions remains a challenge today, we believe that the solution lies in supplying better information to prescribers. Benmedica is on the forefront of creating, reviewing, and augmenting drug coverage information, including alternatives, so that employers and payers can use robust information to ease the physician prescription-selection burden while improving relationships with patients.
If you have questions, contact us to discuss how we can help your organization improve alternatives with our SmartAlts™ service please contact the Benmedica team today.
While real-time pharmacy benefit checks are increasingly touted as the answer to formulary needs within Electronic Health Record systems (EHRs), prescribers and patients often require additional information to develop effective treatment plans. High-quality formulary and benefit data in the EHR can provide complete prescribing information without impacting provider workflow. Formulary and benefit data provides more detail than a single product real-time inquiry by offering comparative data across all products in a therapeutic area.
Benmedica has done significant work with payers to establish processes for ensuring that the right information reaches prescribers at the right time. Based on our experience, real-time pharmacy benefit checks and formulary and benefit data each has its own benefits and limitations.
In most EHRs, providers can use formulary and benefit information to select appropriate, cost-effective medications for patients. Payers can specify formulary statuses, coverage limitations and even tier copay levels in their formulary information for display within the EHR. A routinely performed eligibility check identifies the correct formulary and benefit data to use for the patient.
Advantages of Formulary and Benefit Data
Limitations of Formulary and Benefit Data
Access to real-time pharmacy benefit information is under development with select payers and EHR systems demonstrating value and testing the structure of data transactions. Early results indicate that the information provided is valuable for creating treatment plans but offers a limited number of treatment alternatives.
Advantages of Real-Time Pharmacy Benefit Check
Limitations of Real-Time Pharmacy Benefit Check
While RTPBC is gaining traction as a valuable tool for prescribers, formulary and benefit information can save time and transaction costs when the payer provides high-quality data. “RTPBC was originally designed to be a secondary check of the current formulary and benefit data, not a substitute. It also is used in a different place in the ePrescribing process and work flow. While it adds value, it is not a replacement,” says Tony Schueth, Point of Care Partners. When used to complement formulary and benefit checks, RTPBC information can yield greater insight into the best treatment plan for a particular patient.
Ultimately, providing patient-specific prescription benefit information “at the point-of-prescribing will help improve patient access to medications and also ensure their prescribers are aware of prescription insurance formulary status and less expensive alternatives when appropriate,” says Bernie Monegain, Healthcare IT News. This is a win-win-win situation for payers, prescribers, and patients.
Benmedica assists health plans and payers with optimizing the data sent through Surescripts and other connections to EHRs for use by prescribers. We have deep experience developing processes to best leverage existing data so relevant copay and formulary information, along with preferred alternatives and custom messaging, reach physicians at the time of prescribing.
If you are interested in learning more about the solutions Benmedica has in place to assist payers with delivering the right information at the right time, please contact us or explore our solutions. For updates on our work optimizing payer information for prescriber use, follow us.
Bruce Wilkinson, the founder, and CEO of Benmedica, has leveraged technology to facilitate healthcare since the birth of electronic prescribing and physician connectivity in 2002. Bruce has extensive industry experience with Accenture, Express Scripts, ZixCorp, and CVS Health and continues to lead the development of healthcare standards through NCPDP. You can connect with Bruce on his LinkedIn page.
Exciting changes are coming to NCPDP's Formulary and Benefit Standard (F&B), and we are reviewing the changes here. This update to the existing standard responds to market events like indication-based formulary designs, clearer formulary statuses and price transparency. The new standard incorporates feedback by payers and EHRs (electronic healthcare record vendors) from their use of the current standard named by CMS in 2012.
When we examine the changes in Formulary and Benefit version 53, we identify four stakeholders that will benefit from the enhanced format.

At NCPDP (National Council for Prescription Drug Programs, an ANSI-accredited , standards development organization providing healthcare solutions), the Maintenance & Control work group will vote to accept the proposal by the Formulary & Benefit / Real-time Prescription Benefit task group. The task group is recommending the following dates:
We have placed some of the changes into groups to assist in understanding the nature of the changes. Of course, we have much more detail available as we make plans to help our clients take advantage of these capabilities and assist them with the data support and information needed to leverage the opportunity this new format presents.
New Formulary Statuses
In this new version, the formulary status will move from numbers to text-based formulary statuses to have information be straightforward to physicians. Also, new formulary statuses will exist for when a brand is preferred, (truly) non-reimbursable, non-reimbursable without PA, and when a drug is part of "carve-out" coverage (processed by another party who is not the payer supplying the formulary). In the current standard, formulary status is a numeric field often displayed as a preferred level, with higher numbers being more preferred. This has been confusing to providers who can confuse patient copay tier where lower tiers are best with preferred levels where higher preferred levels are more desirable.
Finally, preferred drugs can now have a separate preference level, which will be consistent with the "lower numbers are better" like patient copay tiers. These changes resulted from the feedback on the current standard collected by the NCPDP Formulary and Benefit Task Group.
Providing formulary information for a drug based on the medication's use is a brand-new addition to the standard. It follows the inclusion of indication-based formulary drug status to Medicare Part D in 2020, mirroring similar commercial plan formularies developments. The indication for medication usually includes something related to the patient's diagnosis or intended use of the drug. Several drug classifications use indication-based formularies. The drug classifications include drugs that treat multiple conditions, but not all the same conditions for all of the drugs.
An example would be TNF alfa inhibitors, which consists of five medications. All five drugs are not approved for all uses of TNF alfa inhibitors. Formularies can now accommodate two medications in a class where Drug A is a preferred drug for psoriasis, and Drug B, in the same classification, is a preferred drug for rheumatoid arthritis.
The current data sorting of which drug is on formulary within a group of drugs for the specific diagnosis usually resulted in prior authorization requirements. Now prescribers will be able to get a view of these more intricate formulary inclusions and exclusions when selecting a medication in their Electronic Health Record system.
Using an indication can also be used for formulary alternatives. For example, Drug C is not preferred, Drug A is a preferred drug for psoriasis and Drug B is a preferred drug for rheumatoid arthritis, the alternatives for each drug use can be displayed separately to make alternatives clearer to providers.

Coverage File Improvements: Drug Alternatives, Step Therapy, Copay, and Prior Authorization Detail
Providing improved coverage information to help prescribers make better choices is a dramatic improvement in the new version.
Drug Alternatives:
Improving drug alternatives with drug use specific alternatives like the indication-based formulary statuses above is another improvement in the new format.
Step Therapy:
There are also improvements in step therapy with new options to communicate more complex step therapy details to prescribers. For example, step therapy will now communicate trials in multiple groups of drugs if required.
Copay:
Improved patient copay information handling creates straightforward capabilities for payers to include patient drug cost information early in the prescribing process.
Prior Authorization:
More information on prior authorization, such as routing, is also an option in formulary data to identify where PA requests should go.
Some drugs are covered under the pharmacy benefit in one plan and covered under the medical benefit in another plan. New information to resolve this issue is in version 53. A method to advise providers can equip providers with plan-specific information in the formulary if a drug is covered in the pharmacy benefit or medical benefit. This improvement can direct providers where to go for more details for cumbersome products that vary where coverage information occurs.
In situations where the provider group is at risk for the total cost of care, including drug spending, formulary data can now include approximate plan drug costs. Using this capability gives providers awareness of drug costs during the prescribing process in their EHR workflow. Risk-sharing agreements have not often included drug costs because there has been no method to communicate costs to providers. This cost transparency will facilitate providers to go at risk with drug cost as part of treatment decisions.
Today providers have no information on what pharmacies are in the network for the patient they are seeing. At times the coverage and patient cost can vary significantly between in-network and out of network pharmacies. The new version of formulary data can include the pharmacy benefit manager's network pharmacy information. Providing network pharmacy information to providers is an essential step in helping the provider get the lowest possible out-of-pocket cost for patients.
There are numerous changes to the file structures to optimize file size, change the structure of headers, and remove unused fields. One enhancement that may help prescribers who don't update formulary files is an expiration date. The EHR can determine if the formulary is outdated and display an appropriate message or even withhold formulary information until the data is updated.
Our team is extensively involved in developing this new version using input and experience in working with our clients. In leading the NCPDP task group, Benmedica has helped drive consensus across the breadth of NDPCP membership. Implementing version 53 requires the creation of new data. It will take effort and time to make the necessary impactful changes at each payer or PBM. Using a knowledgeable team to implement changes, like the team at Benmedica, can provide the required experience and expertise to drive more savings for patients, providers, and payers while shortening the implementation timeline.
We can help payers to plan and implement these changes. We have supplemental data for formulary information like our Smart Alts™ drug alternatives to integrate as required. As part of the process, there may be methods to introduce additional information in 2021 formularies before version 53 becomes commonplace to create a plan and patient savings through better formulary communications. For more information on Benmedica and how we might help your organization transition, contact us here.
Pharmacy Benefit Managers (PBMs), prescribers, and pharmacists all play a crucial but different role in communicating prescription savings opportunities to patients.
PBMs work with their clients to create plan designs and provide data to other parties that drives the electronic prescribing process. In addition, PBMs are beginning to encourage their members (patients) to join the discussion.
Prescribers normally have the ability to access understandable and actionable formulary , copay and coverage information within their Electronic Health Record (EHR) system to guide prescribing decisions for their patients, but frequently the information they receive through their EHRs is limited or unhelpful.
Pharmacists also play a role in the prescribing process by identifying prescription savings opportunities as a “backstop” when prescribers have not recognized them.
Patients are increasingly able to use web portals and apps to understand cost considerations and make more informed decisions about their prescribed treatments.
Having robust, complete, consistent and accurate data throughout the process will enable all stakeholders to achieve reduced drug costs.
This article explores the tools used to communicate drug information to prescribers, pharmacists, and patients, what prescription decision support information is available, and the impact of each tool in identifying prescription savings opportunities.
There are two predominant methods to pass information about drug coverage to physicians, pharmacists, and patients. The first is formulary data to physicians, delivered through their EHRs and the second is largely using adjudication systems to price a drug in real time.
Adjudication systems have been used to process claims in pharmacies for decades. Now these systems are being modified for use by physicians and patients. By combining formulary & benefit with adjudication systems, there are now multiple places where drug benefit information can be accessed: formulary and benefit information (EHRs, mobile/portal) and real-time benefit check information (EHRs, pharmacy claims, mobile/portal).

We review each of these below to better understand the impact on electronic prescribing.
Formulary and benefit data, along with eligibility information, is the first opportunity to communicate drug savings options to prescribers. In most cases, formulary information appears during the prescription-writing process, giving doctors much-needed guidance during drug selection regarding drug coverage, copay and alternatives.
There are several components to formulary data:
Patient Eligibility Information
Patient pharmacy benefit eligibility within the physician’s EHR identifies appropriate formulary information including coverage restrictions and copays for each patient. Eligibility information is currently available for over 90% of insured patients according to Surescripts.
Eighty-six percent of providers in a recent survey indicated that reliable electronic prescribing solutions would benefit their patients and assist them in making more informed prescription decisions.
The patient formulary is generally identified the night before the visit based on the provider’s schedule though it can also be run as part of the patient check-in process for walk-in visits. This ‘eligibility’ check enables the EHR to display appropriate drug specific formulary coverage information during the patient visit automatically.
During the visit, the prescriber’s EHR can display formulary information during drug selection, the first step in the prescribing process. The prescriber can select a drug and see formulary information for similar drugs, providing a more informed view of the patient’s benefit.
Formulary Status and Preferred Drugs
Formulary status is the primary way formulary data conveys drug coverage and preferred medications. Formulary status ranges from not covered, non-formulary/off formulary, on-formulary, and multiple levels of “preferredness” where a higher formulary status value is better. Using preferred levels ranks the most preferred drugs, signaling to prescribers the more preferred on-formulary drugs.
Prior Authorization Indicators
Formulary information can communicate to prescribers that a drug requires prior authorization (PA) for it to be covered under the patient’s insurance. Having accurate prior authorization indicators in formulary data allows prescribers to initiate and submit a PA request electronically, many times right from their EHR.
According to CoverMyMeds, PA requests submitted electronically allow health plans to respond up to three times faster than other submission methods like fax or phone, getting patients their medications sooner. Effective communication of PA requirements allows initiation of the PA request at the point of prescribing, reducing the need for rework and retrospective submission after the patient has gone to the pharmacy.
Drug Alternatives
Formulary data can communicate alternatives to a selected drug. The amount of information provided depends on the payer. Drug alternatives can be vague if poorly selected, like including a first-line generic treatment as an alternative for a more expensive second line brand. We discussed the need for good alternatives in our article, “Automating Alternatives Across a Formulary”.
Well considered and relevant alternatives covering a majority of medications offers a superior way to aid the prescriber in selecting a cost-effective medication for the patient.
Cost Information
Cost information can also be included in formulary data, though it may be limited to the copay tier or, at best, the patient copay amount. There are other factors like deductibles and coverage limitations that might change this amount. Payers can also add additional estimated drug cost messages. This is particularly helpful for health systems at risk for drug costs by helping physicians understand the plan cost of a drug. A future version of the formulary data used in EHR will explicitly support an estimated drug cost range.
Overall, as a physician is reviewing drug options, copay amount or drug cost messaging are excellent inputs to drive savings for patients and plans.
Step Therapy
Formulary data can also indicate that step therapy is required. Payers use step therapy to restrict access to certain drugs until the patient tries another approved drug first.
Step therapy information in formulary data can signal that patients must use other drugs before approval is granted and what specific drugs are included in that requirement. Formulary data provides the background and clarity around these PBM step therapy restrictions.
Formulary data has the potential to be expanded to include critical information prescribers need during patient visits. A recent survey revealed that 3 out of 4 doctors are influenced by drug costs when making a prescription decision.
But formulary information can be perceived as vague if it does not include all applicable coverage indicators. In addition, pricing and insurance information can often be hard for prescribers to locate and even with access to formulary information, its scope is limited.
The information received from Real-Time Prescription Benefit (RTPB) information is similar to what is available in the formulary except that the physician has to enter most information for a complete prescription (including drug strength and form, quantity, and days’ supply) and then select the pharmacy to submit the information. Consequently, the RTPB information is delivered at the end of the prescription writing process.
RTPB transactions return much more precise cost information because the systems treat these transactions as test claims. This allows the system to calculate the patient costs, identify any coverage edits and, in some cases, determine the patient deductible remaining. This information can also include quantity limits, prior authorization requirements, and drug alternatives.
Receiving information at this point in the prescribing process requires the prescriber to create a new prescription for a new medication, leading to some level of rework while the patient is in the office if a change is needed.
Unlike formulary information, which casts a wider net on information returned, RTPB focuses on the drug requested and possibly a few alternatives. In implementations seen so far, prescribers report drug alternatives being available for only a fraction of transactions. The search for a second drug without alternatives requires another attempt that might find a less expensive alternative or a drug without a prior authorization, or it may not.
Sometimes prescribers have selected the best option and do not require a drug alternative to save the patient money. Other times there are potential alternatives that aren’t (yet) provided by the PBM. Drug alternatives are not required in RTPB information returned to physicians and patients. Still, RTPB information represents a significant opportunity to communicate savings to physicians.
Yet much of real-time information has yet to make an impact. A recent survey from CoverMyMeds revealed that nearly half of providers indicated that they never have out-of-pocket medication price information available at the time of prescribing, even though 80% say patients are requesting this information.
After receiving the prescription, the pharmacy staff processes the prescription and submits a claim for payment. As part of the claims process, PBMs communicate patient drug costs, deductibles, prior authorization requirements, and quantity limits.
Drug alternatives may also be included as part of the claims process to assist in identifying options for patient savings. This represents the last opportunity for a drug alternative suggestion and is the final point before the prescription is dispensed.
If there is a savings opportunity that requires a prescription change, the pharmacy staff may need to contact the physician to obtain a revised prescription. Revising a prescription usually requires rework by both pharmacy staff and the prescriber and may result in delays in the patient starting treatment.
Keeping patients updated on their benefits and the cost of prescriptions is an ongoing challenge. Patients are more eager than ever to engage in treatment decisions and include cost as part of those decisions. Help is available in the form of health plan member-facing web portals and apps.
These websites and apps provide drug price transparency information, indicate if prior authorization is required, include quantity limit information, and suggest available drug alternatives.
Prescription cost information is useful before and during an office visit and somewhat less useful retrospectively. When a patient does not have access to cost prior to visiting their pharmacy, they are more likely to abandon expensive drugs or request a new, more affordable prescription.
Along with those health plan websites is a growing number of apps from tech startups that include the ability to compare prices across local pharmacies both through benefits and cash prices.
The bottom line is that patients should be involved in the prescription decision-making process, particularly where cost considerations are a factor. Patients should know what they’re expected to pay and what their other options are at the point of prescribing. This ultimately saves time and lowers drug costs for everyone involved.
The Common Denominator: Using Formulary Information to Improve Prescription Decisions
While RTPB capabilities are often touted as the solution to information gaps, too often inaccurate and incomplete data, including drug alternatives, are provided after the provider has already input all the required information to prescribe a drug. The information returned by real-time checks can be narrow, offering few options for lower cost, therapeutically similar alternatives. This results in more burden on physicians for rework to resolve issues.
But the good news is that an end-to-end solution exists today that addresses all stakeholder needs and is already implemented in physician EHRs. Taking time to enhance and augment existing formulary and benefit data PBMs provide today is needed to keep the different data sources in sync and communicate savings opportunities in as many methods as possible.
To learn more about how easy and quick it is to enhance your formulary information and realize estimated savings of up to $167 per member per year (or more!), contact the Benmedica team today.
Congress mandated that Medicare Part D plans provide patient cost information to physicians in their EHRs. These Real Time Benefit Tools (RTBT) have been rolled out to physicians through various EHR system updates. A study published in November 2022 in the Applied Clinical Informatics raises questions about the usefulness of RTBT information to physicians if the information does not appear in the optimal time during a physician encounter.
In addition to physician concerns about the overall accuracy of the information, the study identified that the information appeared late in the patient encounter after the drug selection discussion with the patient. This underscores the need for payers and PBMs to not only support Formulary and Benefit (F&B) information in the EHR but to enhance their existing support if they already provide it to inform early drug selection.
The study included 15 semi-structured interviews of prescribers of high-cost medications getting feedback on the physician experience with patient cost information in their EHR. While some may say that the small sample size limits the usefulness of the insights, the researchers determined that the redundancy in the responses did not require additional interviews. The major themes were identified, and additional interviews would underscore existing insights
Patient cost is a complex topic and the physicians interviewed expressed concerns about the accuracy of the information presented and the format of the information. Other cost information reference sources contained approximate patient costs or overall medication costs. Neither of which were useful in identifying the best medication for a patient. Additionally, the method that information is displayed can be confusing and may require a cost discussion with the patient. Often physicians do not have experience with these types of cost discussions.
The study included four use cases for patient cost information during a visit:
We would add one other use case for RTBT. RTBT can also include information on Prior Authorization requirements specific to a patient. For some more sophisticated payers, the incoming request can be triaged to determine if prior authorization is required. For example, if there is a prior authorization in place because the patient needs to have tried and failed on a less expensive drug (step therapy), the payer can identify that the patient has met the criteria and remove the prior authorization requirement for that patient. This could lower the prior authorization burden for patients who meet the payer requirements for m medication.
Physician interviews centered on two times during a patient encounter where drug cost information might be useful. First is during order entry, when it might be most immediately actionable before a discussion of medication options with a patient. The second is during prescription entry before the order is completed.
The workflow as it has been established requires that the physician complete entry of the entire prescription including the quantity and the intended pharmacy. This is after the discussion with the patient about the medication and requires rework to change a prescription.
As we pointed out in our whitepaper, Physician Insights into Formulary Accuracy, Usability and Real Time Pharmacy Benefit Information, RTBT adds to the physician burden through (1) the time involved to review data from real-time checks on every prescription and (2) how far into the process of writing a prescription they were before a real-time check confirmed a choice or required a change.
Formulary & Benefit (F&B) information is present in EHRs when a drug is being selected during order entry. That is the precise time when cost information is of the most value. F&B provides guidance on a drug’s formulary status, prior authorization or other coverage alerts, copay and potential drug alternatives. This is available immediately during drug selection which helps the prescriber write the optimal prescription before triggering a RTPB transaction. RTBT is used as verification, confirming patient-specific coverage alerts and providing drug prices (both for the originally selected drug and potential alternatives at the specified pharmacy.
There are some limitations to formulary data that should be recognized:
There are delays in updates but there are also new services to access formulary data from Surescripts and others that do not require periodic downloads and updates. Providing F&B data as a web service can eliminate update these delays. Surescripts does offer a service to provide F&B data in real time, reducing delays because of an update process.
How Benmedica Can Help
Benmedica is on the forefront of creating, reviewing, and augmenting drug formulary, copay and coverage information so that employers and payers can use robust information to ease the physician prescription-selection burden while improving relationships with patients. Not only will patients be able to take their medications more quickly, they will also typically be less expensive. Benmedica can also tie together the drug alternatives from F&B & RTPB to provide a more consistent experience.
If you have questions, contact us to discuss how we can help your organization improve F&B and RTBT please contact the Benmedica team today.
In a recent article, we compared the drug alternatives information provided by seven Pharmacy Benefit Managers (PBMs) to understand how useful that information is for supporting prescription decisions.
We noted that there are several areas where improving the data provided or the mechanism for communicating alternatives, can save all stakeholders – physicians, patients, pharmacists, and PBMs – time and money.
In this article, we lay out best practices for PBMs to adopt when providing alternatives information. Our hope is that by adopting these best practices, PBMs will take a step forward in improving patient outcomes, and greater savings for all stakeholders.
Alternatives are in place to help providers and their patients choose the optimal medication that meets the patient’s needs. Available options may vary from one insurance plan to another based on the patient’s cost for the drug (copay or drug cost if a deductible has not been reached) and prior authorization requirements. Alternatives offer a method for PBMs to suggest to providers and patients other more preferred medication options.
Before we delve into the best practices themselves, let’s take a quick look at why providing alternatives information within formulary or real-time pharmacy benefit information in EHRs and in patient facing tools is so critical.
According to a CoverMyMeds survey, as many as 50% of patients abandon prescriptions because of price.
Access to alternatives information, lets doctors know what other more cost-effective or covered options are available. This can slash prescription abandonment and potentially save PBM clients over $167 per member per year1. In addition, it reduces patient out-of-pocket drug costs.
Below are the best practices PBMs can adopt to increase their savings on drug costs as well as reduce patient costs.
1. Systematically identify all opportunities to provide alternatives
Directing physicians to similar but lower cost drugs is an unparalleled opportunity to create patient and payer savings. Yet many PBMs only provide alternatives for only a small subset of drugs.
PBMs can look among groups of drugs with the same indications to identify which drugs have alternatives that can save the patient money on their copay or out-of-pocket costs. A process should be established to identify drugs that have a better formulary alternative or a lower copay option in the therapy area.
Alternatives should be included in formulary data, in real-time pharmacy benefit data sent to providers’ EHRs, and in patient portals or plan websites. It is important that alternative data be consistent across these areas so as not to inadvertently create any confusion.
2. Identify relevant alternatives with appropriate strengths
All drugs in the same classification are not always alternatives for each other at the selected dose.
For example, the statin Livalo available in a 4 mg tablet has available alternatives in the market but none are 4 mg.
To help doctors identify other options, therapeutically similar doses should be included in alternatives drug listings.
3. Drugs not covered should have alternatives (whenever possible)
When a drug is not covered by the PBM there should be alternatives listed for the drug. This can’t be done if the entire category of drugs is excluded from coverage (e.g. drugs for hair growth).
For drug classes that do have covered options, PBMs can promote better patient outcomes while saving money by offering alternatives.
4. Prior authorized drugs should include lists of alternatives
Many formulary lists on PDFs and websites include prior authorized drugs with a side-by-side listing of the alternatives. Displaying alternatives is a bit more complicated in EHRs and patient websites. Prior authorized drugs and those with other restrictions like step therapy should have non-prior authorized, relevant alternatives included.
When doctors don’t have access to alternatives for restricted drugs, they are left to guess what options might meet their patients’ needs. For payers, this drives up drugs costs because doctors may select another drug that is less cost-effective. For patients, the chance of prescription abandonment increases due to cost.
5. Only less expensive options should be included
The decision process shouldn’t include all drugs in the therapy area. Care should be taken to list only alternatives that are less expensive than the target drug.
In our review of the data provided, we found that in some cases, PBMs provided alternatives that were more expensive than the selected drug. This obviously doesn’t help doctors make cost-driven prescribing decisions.
6. Only relevant alternatives should be included
Deciding which alternatives to include is certainly subjective. Including drugs most physicians have already considered or the patient has tried and failed is not helpful.
For example, suggesting sumatriptan as an alternative to the newer and more expensive migraine prevention drug Aimovig® is not relevant for patients who need to prevent (instead of treat) migraines. While the patient would save with the decades’ old treatment, it treats existing migraines and does not prevent them.
There are drugs that have multiple uses. These can be the most difficult to discern alternatives. Careful attention needs to be paid to these drugs to provide relevant information to providers.
For example, alternatives for Humira would require a better understanding of the indication involved as not all of the alternatives are approved or used for every indication.
7. Use appropriate resources in creating alternatives
Developing drug alternatives using drug compendia classifications can lead to providing too few alternatives, too many alternatives, or possibly inappropriate alternatives. This could result in displaying alternatives options to doctors that are not therapeutically useful.
Without taking the time to enhance drug alternatives information using the right tools and experience, prescribers waste precious clinical time with patients sifting through alternatives and payers lose the opportunity to guide prescribers to cost-effective options.
8. Widely distribute alternatives
Providers and patients are both looking for improved information to assist in selecting medications that patients can afford and are effective. While 87% of physicians receive formulary information through their EHRs, this information needs to be improved so it offers actionable prescribing guidance to doctors.
Emerging tools like real time pharmacy benefit information in EHRs and in health plan apps for patients represent new opportunities to communicate with prescription decision makers. Without including accurate, enhanced, and consistent alternatives data, these new sources of information will not work at their full potential to maximize cost-saving drug suggestions to prescribers and patients.
This means that payers must improve the information to help prescribers identify cost savings.
We are in a period where formularies are getting more and more restrictive. Because of this, providers need additional direction to navigate ever more complicated and changing drug benefit restrictions and formularies.
Formulary information in EHRs provides an important channel to communicate with physicians during drug selection. The newer real-time pharmacy benefit tool provides another opportunity to inform physician decisions to the most cost-effective drug, although it occurs at the end of the ePrescribing workflow.
But this opportunity needs to be widely adopted. The frequency of alternatives is just as important as the relevance of the alternatives shown. In many cases prescribers will need to make some effort, like selecting a button, to find these alternatives in their EHR. If the data remains scant, as our small sample indicated, prescribers may abandon their pursuit of alternatives.
We have entered an age of consumerism in healthcare where patients are seeking cost information to be part of the drug decision process. Patients too need guidance to select the most cost-effective treatments to have more meaningful discussions with their physicians.
Benmedica’s Experience with SmartAlts
Benmedica has generated drug savings for over 15 million lives, helping capture part of the savings potential of over $167 per member per year. Drug alternatives play a critical role in creating savings by providing valuable and actionable information to prescribers during the decision-making process.
Consumers too need assistance and guidance in choosing cost-effective drugs. Benmedica’s SmartAlts system can customize alternatives for any drug benefit. Health plans too can supplement their PBM information with alternatives to create additional savings and can share the information via multiple channels – to prescribers, patients and pharmacies.
Our goal is to drive significant drug savings for payers, PBMs and members by unlocking the savings potential of alternatives - reach out to us to start the discussion.
A recent announcement from the Centers for Medicare & Medicaid (CMS) has opened the door for Medicare Part D plans to use indication-based formularies beginning in 2020. This policy expansion provides a new tool for Part D plans to leverage costs and communicate formulary status to better inform prescribers and patients while solidifying what commercial payers may have been doing all along by using Prior Authorization (PA).
Today’s formularies only allow a drug to have a single formulary status indicating whether the drug is covered and, if it is covered, how preferred the drug is on the formulary. A drug covered for one indication must also be covered for all indications approved by the Food & Drug Administration (FDA). This forced payers to either require a prior authorization for a drug (and approve selected uses) or cover a drug across all uses.
Indication-based formularies allow payers to communicate drug coverage based on the condition for which it is being prescribed. Instead of approving or denying coverage by the drug, payers can design their formularies to include drugs for certain indications and not for others. Any indication not approved would require the prescriber or patient to follow the same process as they would for other off-formulary drugs.
While designing formularies with specific indications in mind is not a new strategy in formulary management, the CMS policy expansion provides payers with an opportunity to bring their indication coverage data into the forefront and make it more readily available to prescribers. As Part D indication-based formularies gain momentum and become more routine, payers will need to communicate indication specifications to prescribers and patients through Formulary and Benefit (F&B) data. These new policies in Medicare Part D will likely expand into other payers’ lines of business as well.
The main benefit of opening Part D up to indication-based formularies is the negotiating power it gives to plans to control drug costs. “[Providing] Part D plans with the flexibility to employ the latest formulary tools would enable them to better negotiate for prescription drugs, especially high-cost drugs. The ability to exclude drugs from their formulary for specific indications will provide additional negotiating leverage with manufacturers, which can ultimately reduce beneficiary and program costs,” notes the CMS memo.
When payers communicate their indication restrictions to prescribers through F&B data in the Electronic Healthcare Record (EHR), prescribers can initially select better prescription medications in their preferred workflow. Choosing the best alternative in the initial prescription avoids callbacks and changes due to uncovered drugs. Under this policy update, Part D enrollees are expected to have better access to medicines and enjoy lower costs.
There may be benefits to prescribers and patients within the commercial sphere as well. Medications that would require prior authorization to identify the indication may appear in formularies as approved for one indication and restricted for another use. Eliminating unnecessary prior authorizations may make medications more likely to be prescribed and therefore more accessible to patients.
There are three initial hurdles to successfully communicating formulary indication restrictions through EHRs: 1) adding indications to formulary statuses, 2) displaying alternatives by indication, and 3) communicating indications.
Adding the Mechanism for Communicating Indication Restrictions
As the governing body of electronic prescribing standards, the National Council for Prescription Drug Programs (NCPDP) has proposed adding three indication fields to Formulary and Benefit (F&B) data as part of the general information section. These fields would include (1) an Indication Code used by the payer to represent the indication, (2) an Indication Code Qualifier to determine code type, and (3) an Indication Code Description that enables clarifying information to be added in the form of free text descriptions.
This flexibility allows payers to modify all F&B elements based on the indication and provides support until the industry can rely on a common indication code vocabulary. If there is no indication, the fields can be left empty.
Another challenge to communicating indication-based formulary restrictions through EHRs is implementing a way for prescribers to find covered alternatives. With a major formulary overhaul such as this, there is increased importance on having alternatives available within formulary data to provide guidance on more appropriate treatments. Actionable alternatives information minimizes prescriber and patient frustration and decreases the occurrence of therapy abandonment.
Payers can curtail these difficulties by expanding alternatives information within their formularies and enabling this data to be displayed through EHRs. If a diagnosis code is known, an EHR would be able to display the clinically appropriate alternatives list.
Nomenclature using ICD-10 and SNOMED CT provides the ability to link a drug to its indication using recognized clinical terminology. However, drug use might not relate to the primary diagnosis of a patient. For example, an oncology patient undergoing chemotherapy might receive an anti-emetic to prevent chemotherapy-induced nausea but not be given a corresponding diagnosis.
ICD-10 codes are primarily used to indicate a diagnosis for reimbursement purposes. Not every diagnosis is documented for a patient, especially when it doesn’t impact reimbursement or treatment. Requiring a diagnosis to meet indication formulary specifications places an additional burden on prescribers to determine and record the patient’s condition.
SNOMED-CT codes can be associated with the prescription and sent to the pharmacy as part of prescriptions. Inclusion of indication information can be used to remind the patient why they should take a particular medication. Every prescription typically has a reason for its use even if the diagnosis isn’t yet documented
Benmedica has begun work to upgrade its systems to add the capabilities for indication-based formularies. Included in this work is the ability to read and send F&B data, develop therapy areas where indication-based formularies may offer opportunities for savings, and supplement existing formularies with relevant alternatives using Benmedica SmartAlts™ technologies.
The NCPDP Formulary & Benefit Task Group, led by Benmedica founder Bruce Wilkinson, has initiated the process of including indications as part of statuses, tiers, copay, prior authorization, step therapy, and medication alternatives. NCPDP members and non-members can participate in Task Group calls (NCPDP.org).
More information on how Benmedica can help payers prepare for and address indication-based formularies is available at Benmedica.com or by contacting Bruce.
Liz Shea, Chief Clinical Officer of Benmedica, holds a BS degree in Pharmacy. Her experience includes retail pharmacy and working as a senior advisor in Product Development for CVS Caremark's physician connectivity area. She has been involved in all aspects of e-prescribing, including formulary & benefit, for over 15 years and continues to work towards improving technology within healthcare.